Integrating Clinical and Laboratory Markers to Predict Transfusion in Pediatric Trauma Patients
DOI:
https://doi.org/10.4274/jpea.2025.464Keywords:
Pediatric trauma, blood transfusion, predictive biomarkers, intensive careAbstract
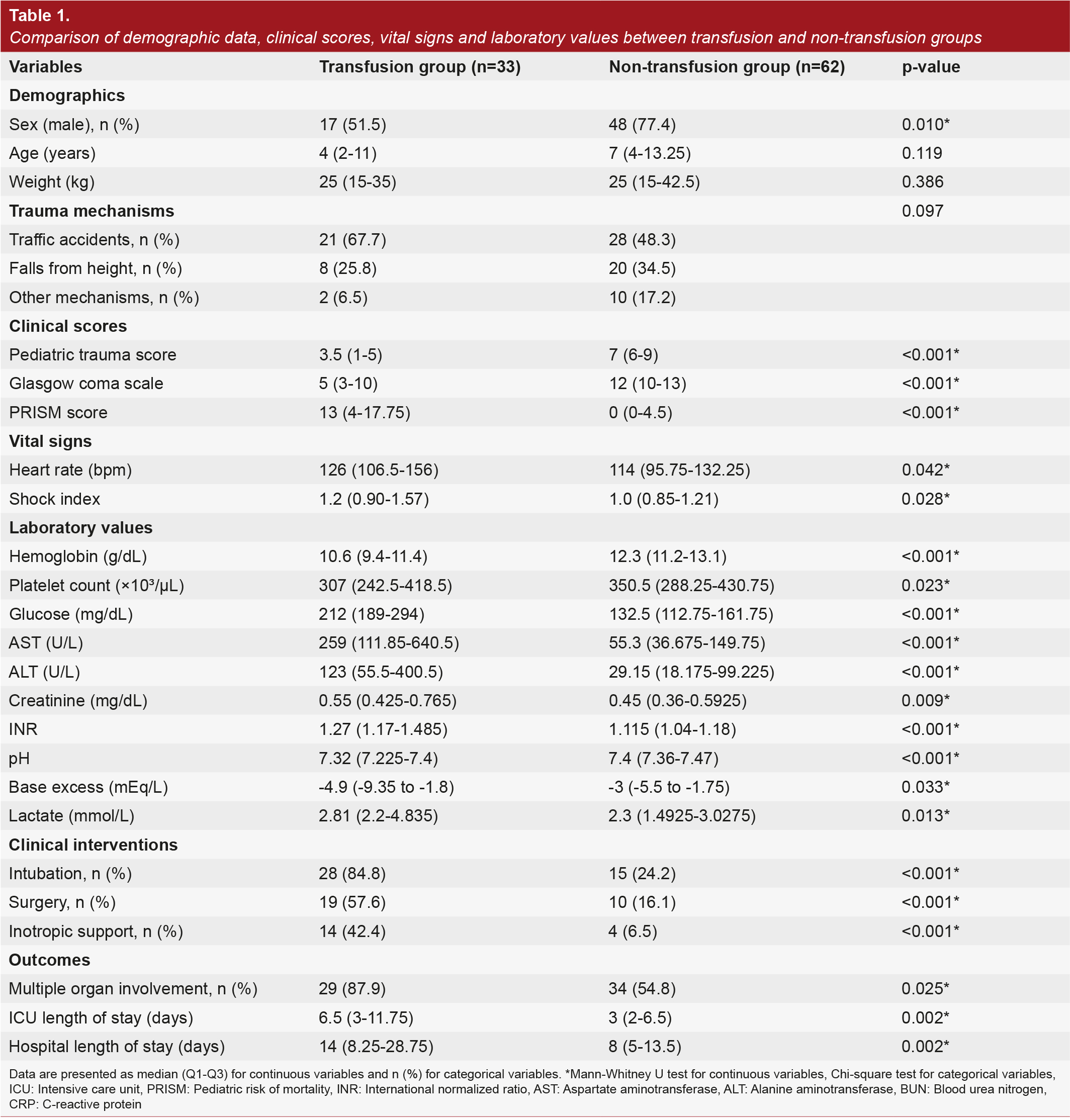
Trauma-related hemorrhage represents a leading contributor to avoidable deaths in pediatric patients and often necessitates prompt transfusion decisions. Unlike adults, children may maintain hemodynamic stability until significant blood loss occurs, making early recognition of transfusion needs particularly challenging. This investigation sought to determine dependable clinical and laboratory predictors of blood transfusion during the initial 24-hour period of pediatric trauma and to establish a practical risk stratification tool to aid emergency decision-making. This retrospective study included pediatric trauma patients under 18 years of age who were admitted to a Pediatric Intensive Care Unit. Clinical and laboratory data at admission were recorded, and patients were grouped based on whether they received blood transfusions during the initial 24-hour period. Univariate and multivariate logistic regression analyses were conducted to determine independent predictors. Receiver operating characteristic curve analysis was employed to establish optimal threshold values and develop a combined risk score for transfusion prediction. Among 95 pediatric trauma patients, 34.7% required blood transfusion within 24 hours. Transfused patients had significantly lower pediatric trauma scores, higher glucose levels, lower platelet counts, and were more frequently intubated. Multivariate analysis identified intubation, glucose, and platelet count as independent predictors of transfusion. A combined risk score incorporating these variables demonstrated high discriminative ability (area under the curve=0.831). Risk stratification revealed transfusion rates of 3.8% in low-risk patients, 30.2% in moderate-risk patients, and 100% in high-risk patients. The combination of intubation, glucose, and platelet count provided a simple yet effective tool for predicting transfusion needs in pediatric trauma. The resulting risk score outperformed individual parameters and allowed for early identification of high-risk patients. This model may help guide timely transfusion decisions and optimize care in emergency settings. Prospective validation is warranted to confirm its clinical utility and broader applicability.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 The Journal of Pediatric Academy

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.